- What Are Croup Symptoms?
- Common Croup Symptoms to Watch For
- Causes of Croup
- Diagnosing Croup Symptoms
- Treatment Options for Croup
- When to Seek Medical Attention for Croup
- Conclusion
Recognizing and Managing Croup Symptoms in Children
What Are Croup Symptoms?
Croup symptoms predominantly affect young children, particularly those aged between six months and three years. It is a common respiratory illness characterized by inflammation and swelling in the upper airway, especially around the vocal cords and windpipe (trachea). This inflammation causes narrowed airways, resulting in distinct respiratory symptoms. The condition typically arises from viral infections, with parainfluenza viruses being the most frequent culprits. Although most cases are mild, croup can occasionally lead to serious respiratory distress requiring immediate medical attention.
Common Croup Symptoms to Watch For
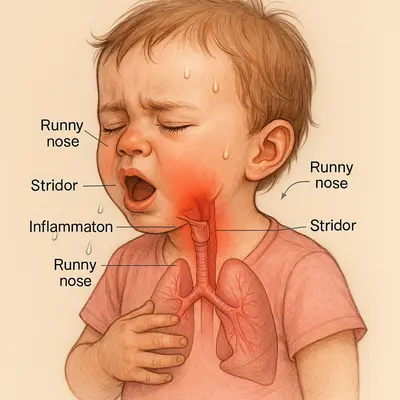
Recognizing the hallmark signs of croup early on can help manage symptoms promptly. Key croup symptoms include:
- Barking Cough: A characteristic harsh cough resembling a seal’s bark, often alarming parents. This cough results from airway swelling and tends to worsen with crying or agitation.
- Stridor: A high-pitched whistling or wheezing sound heard during inhalation, indicating significant narrowing of the child’s airway.
- Hoarseness: A raspy or rough voice due to inflammation around the vocal cords.
- Fever: Usually mild, but severity can vary depending on the viral cause and individual immunity.
- Runny Nose and Congestion: Commonly precede the more prominent respiratory symptoms, resembling a typical cold.
- Difficulty Breathing: In severe cases, children may exhibit signs such as rapid breathing, chest retractions (the chest visibly pulling inward during inhalation), and nasal flaring.
Symptoms generally become more pronounced at night, potentially causing significant distress and anxiety for both the child and parents.
Causes of Croup
Croup is predominantly viral in origin. Parainfluenza viruses are responsible for approximately 75% of cases. Other common viruses include:
- Influenza A and B Viruses: Capable of causing severe cases, especially during influenza seasons.
- Respiratory Syncytial Virus (RSV): Frequent in young children, potentially causing additional complications such as bronchiolitis.
- Adenovirus: A less common but important contributor to respiratory infections leading to croup.
- Measles Virus: Rarely associated, primarily in populations with low vaccination rates.
Bacterial causes are uncommon but can occasionally complicate viral infections, leading to conditions such as bacterial tracheitis, which requires prompt medical intervention.
Diagnosing Croup Symptoms
Healthcare professionals typically diagnose croup clinically based on the child’s distinctive symptoms and a physical examination. Laboratory tests and imaging studies like X-rays are generally unnecessary unless the child presents atypical features or severe symptoms requiring further evaluation.
Treatment Options for Croup
Effective management of croup depends on symptom severity and includes:
- Mild Cases: Most children recover well with simple home care. Keeping the child calm, providing adequate hydration, and monitoring symptoms closely is essential. A humidifier or cool air exposure may occasionally help ease breathing.
- Corticosteroids: These medications significantly reduce airway inflammation. Oral or injectable steroids, like dexamethasone, are effective in decreasing symptom severity and shortening illness duration.
- Nebulized Epinephrine: Reserved for moderate to severe cases, epinephrine quickly relieves airway obstruction by reducing swelling around the vocal cords and upper airways. It provides temporary relief and is often used alongside steroids.
- Hospitalization: Necessary for severe cases, particularly those involving persistent breathing difficulties or oxygen deficiency.
When to Seek Medical Attention for Croup
Immediate medical care is crucial if your child exhibits any of the following symptoms:
- Stridor at Rest: Indicates severe narrowing and possible blockage of the airways.
- Difficulty Breathing: Rapid breathing, noticeable chest retractions, and signs of exhaustion.
- Bluish Skin Color (Cyanosis): Particularly around lips, mouth, or fingernails, suggesting insufficient oxygen.
- Drooling or Difficulty Swallowing: Could indicate a severe complication like epiglottitis, requiring urgent medical intervention.
- Lethargy or Decreased Responsiveness: May indicate inadequate oxygenation or significant distress.
Preventing Croup
Implementing prevention strategies can significantly lower the risk of croup:
- Vaccinations: Ensure your child receives recommended vaccinations, including those against influenza and diphtheria, to minimize severe respiratory infections.
- Hand Hygiene: Regular handwashing with soap and water or alcohol-based hand sanitizers reduces viral transmission.
- Avoiding Sick Contacts: Limit your child’s exposure to individuals with respiratory infections, particularly during peak cold and flu seasons.
- General Health: Maintain good overall health and nutrition to support a robust immune system capable of fighting viral infections.
Conclusion
Being well-informed about croup symptoms is essential for early detection, appropriate management, and preventing complications. While croup is generally manageable and self-limiting, vigilance and prompt medical care are crucial in severe cases to ensure the child’s rapid recovery and overall well-being.
The following posts may interest you
When Should I Worry About a Baby’s Cough?
Croup Cough: Understanding and Managing It in Children
Sources
Croup: An Overview
https://www.aafp.org/pubs/afp/issues/2011/0501/p1067.html/a
Symptoms and signs differentiating croup and epiglottitis
https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1440-1754.2010.01892.x
Outdoor Cold Air Versus Room Temperature Exposure for Croup Symptoms: A Randomized Controlled Trial
Observations on Croup:—Symptomatography
https://pmc.ncbi.nlm.nih.gov/articles/PMC5315157
Croup in Children (Acute Laryngotracheobronchitis)