- Diabetic Ketoacidosis: Understanding the Condition and Its Management
- What Causes Diabetic Ketoacidosis (DKA)?
- Symptoms of Diabetic Ketoacidosis (DKA)
- Diagnosing DKA
- Preventing DKA
- Complications of DKA
Diabetic Ketoacidosis: Understanding the Condition and Its Management
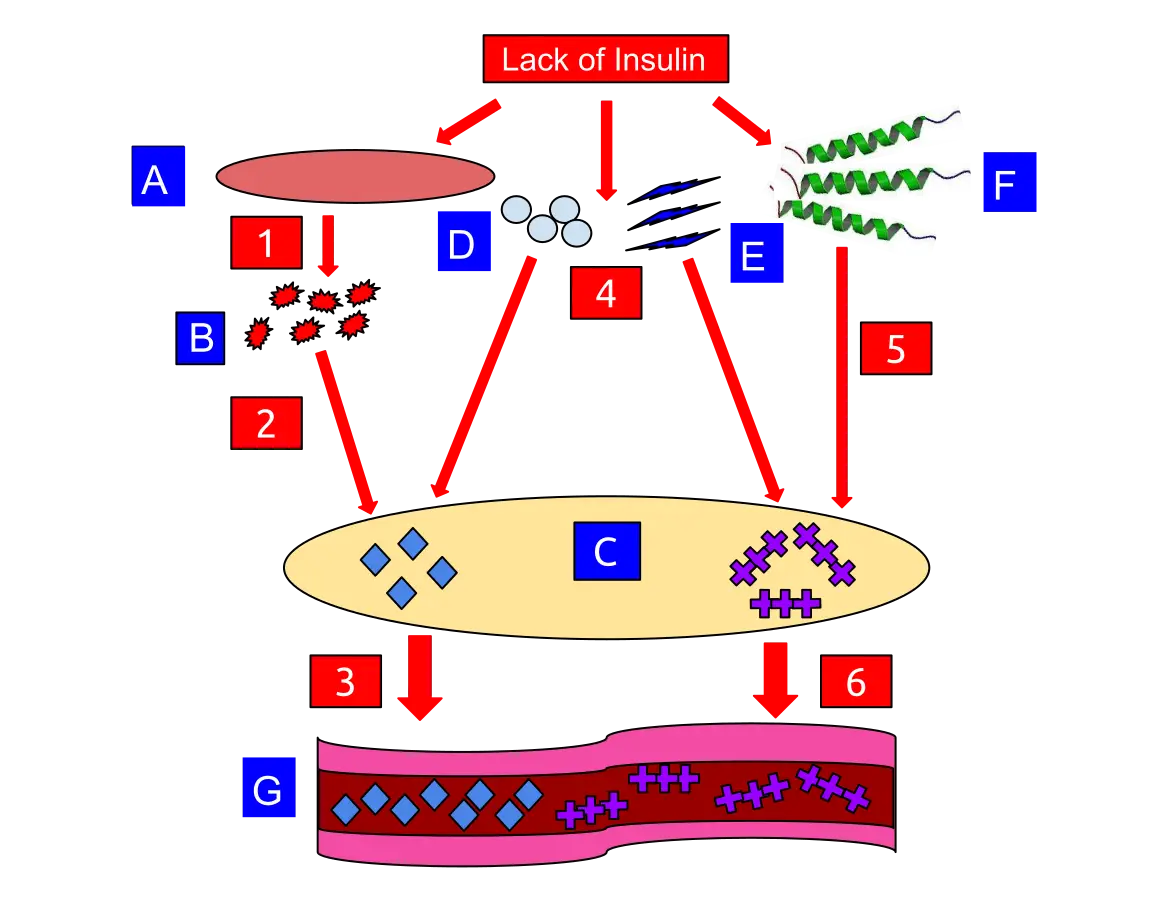
Diabetic ketoacidosis (DKA) is a serious and potentially life-threatening complication of diabetes. This condition occurs when the body cannot produce enough insulin, a hormone essential for regulating blood sugar levels. Without sufficient insulin, the body begins to break down fat as an alternative energy source, leading to the accumulation of acids called ketones in the bloodstream.
What Causes Diabetic Ketoacidosis?
DKA usually develops in individuals with type 1 diabetes but can also occur in those with type 2 diabetes under certain conditions. Common triggers include:
- Infection or illness: Infections or illnesses can cause the body to produce higher levels of certain hormones, such as adrenaline or cortisol, which work against the effects of insulin.
- Missed insulin doses: Skipping insulin treatments or not taking enough insulin can lead to a deficiency.
- Physical or emotional stress: Stressful situations can increase the demand for insulin, sometimes resulting in DKA.
Symptoms of Diabetic Ketoacidosis
The symptoms of DKA often develop quickly, sometimes within 24 hours. Key symptoms include:
- Excessive thirst and frequent urination
- Nausea and vomiting
- Abdominal pain
- Weakness or fatigue
- Shortness of breath
- Fruity-scented breath
- Confusion
Diagnosing Diabetic Ketoacidosis
Diagnosis typically involves a combination of clinical evaluation and laboratory tests. Doctors look for high blood sugar levels, high ketone levels in the urine or blood, and acidosis indicated by a low pH in the blood. Symptoms such as rapid and deep breathing (Kussmaul respirations) are also indicative of DKA.
Treatment and Management
Treating DKA involves addressing the underlying causes and correcting the body’s biochemical imbalances:
- Fluid replacement: Intravenous fluids help rehydrate the body and dilute excess sugar in the blood.
- Electrolyte replacement: DKA often results in the depletion of important electrolytes like sodium, potassium, and chloride. These need to be replenished to ensure proper bodily functions.
- Insulin therapy: Administering insulin helps reduce blood sugar levels and halt the production of ketones.
Preventing Diabetic Ketoacidosis
Effective diabetes management is key to preventing DKA. Here are some preventive measures:
- Regular monitoring: Check blood sugar levels frequently, especially when feeling unwell or under stress.
- Adherence to insulin therapy: Take insulin as prescribed and never skip doses.
- Stay hydrated: Drink plenty of fluids to help prevent dehydration.
- Healthy lifestyle: Maintain a balanced diet and engage in regular physical activity.
Complications of Diabetic Ketoacidosis
While DKA is treatable, it can lead to severe complications if not addressed promptly:
- Cerebral edema: Swelling in the brain can occur if the blood sugar level drops too quickly.
- Low potassium levels: Insulin therapy can cause potassium levels to drop, potentially leading to heart and muscle issues.
- Hypoglycemia: Overcorrection of blood sugar levels can result in dangerously low blood sugar.
Sources
https://www.aafp.org/pubs/afp/issues/2013/0301/p337.html
https://www.nature.com/articles/s41572-020-0165-1
https://www.cmaj.ca/content/168/7/859.short
https://www.acpjournals.org/doi/abs/10.7326/0003-4819-152-1-201001050-01001?journalCode=aim
Foto:
https://en.wikipedia.org/wiki/Ketoacidosis#/media/File:Diabetic_Ketoacidosis_Model.svg